To hear Jennifer Perkins say it, losing her health insurance would be a real nightmare.
Like nearly 25% of people with diabetes, Perkins has had to ration his insulin, a dangerous practice that can potentially lead to blindness, kidney failure or even death. Yet the out-of-pocket expense of the drug forced her to rely on a supply from a friend’s grandmother to carry her through.
“Grandmas can’t be our state’s emergency insulin program,” said Tacoma nurse Perkins.
A bill, which was passed by the State Senate last week, would reduce the cost of insulin in Washington. If passed into law, Senate Bill 5546 would set a copayment cap of $35 per 30-day supply of the drug for all participants in state-regulated insurance plans, such as Medicaid and state employees. This would not apply to private health insurance plans.
The bill went through a public hearing in the House Committee on Health Care and Welfare on Thursday and House Majority Leader Pat Sullivan, D-Covington, said called the bill’s chances in the chamber “very good.”
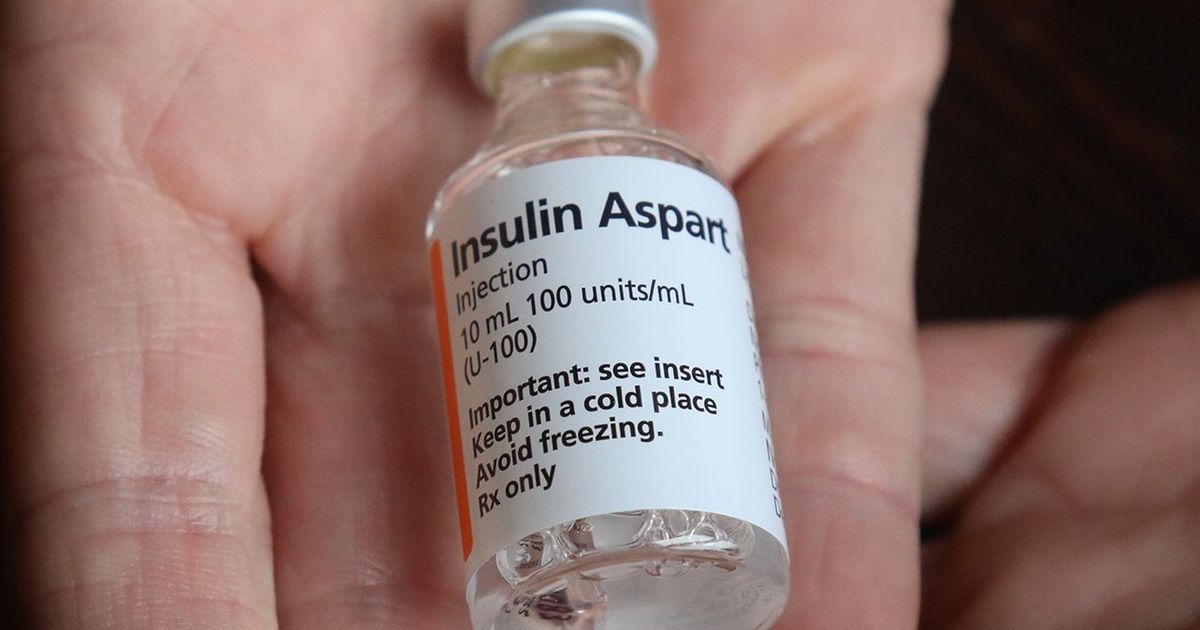
Nearly 1 in 8 adults in Washington live with diabetes and about 1 in 3 use insulin, according to the state Department of Health. A hormone produced by the pancreas, insulin helps the body to transform the sugars and carbohydrates contained in food. People with type 1 and type 2 diabetes have trouble producing or processing insulin, making the drug essential for survival. A 2019 DOH report identified diabetes as the seventh leading cause of death in Washington.
“Insulin is a life or death drug. We know people have died because they couldn’t afford insulin,” said the bill’s lead sponsor, the Sen. Karen Keiser, D-Des Moines, during her January 19 public hearing.
Currently, 18 states have legislation capping insulin co-pay costs, and the issue has recently gained national attention. President Joe Biden’s Build Back Better program includes measures that would cap insulin copayments at $35 per 30-day supply for some Medicare patients. The bill was passed by the US House of Representatives in November and is currently being negotiated in the Senate.
But self-funded group insurance plans, the most common types for large corporations, fall outside the state’s regulatory jurisdiction and therefore would not be subject to the new bill or its co-pay caps. About 3 million Washingtonians, or less than half the state, are enrolled in health plans that would qualify for the $35 copayment cap, according to figures from Democratic Senate and State Health political staff. Care Authority.
Many Washingtonians with diabetes say the state bill doesn’t do enough to address the root of the problem: complicated insurance plans and pharmaceutical companies benefiting from inflated insulin prices. . According to the DOH report, the total cost of diagnosed diabetes in Washington was $6.7 billion in 2017.
“Having this experience where you’re at your pharmacy counter and they have the life-saving medicine you need on the other side, and you can’t get it… It will make anyone cry,” said Perkins. “You just need it.”
Diabetes advocates say price caps, as opposed to co-pay caps, are a more effective way to increase insulin affordability by limiting all patient out-of-pocket costs, regardless of type of drug. insurance they have.
“Setting how much insulin can be sold would really affect people with or without insurance,” said Madi Johnson, Washington chapter leader of #insulin4all, a volunteer advocacy group.
Sen. Mike Padden, R-Spokane Valley, the committee’s only negative vote, raised concerns about the government’s attempts to set insulin price limits.
“As someone with a family history of diabetes, I am very sensitive to the need for affordable access to insulin. I am also very supportive of efforts by pharmaceutical companies to provide insulin at affordable prices. discounted or free. But experience has proven time and time again that price controls don’t work,” Padden said in an emailed statement. “Big government is almost never the right answer.”
In 2020, the Legislature passed Senate Bill 6078, setting a $100 disbursement limit and establishing the Total Cost of Insulin Task Force, which was charged with creating strategies to reduce costs. insulin. The $100 cap, which expires at the end of this year, was intended to serve as an interim measure to give the task force time to find a more permanent solution, although the pandemic prevented the group from meeting before the end of the year. expiration of its funding.
Another bill, House Bill 1728, would again fund the task force, although some of its supporters are calling for amendments. They point out that of the 14 representatives of the group, seven of them would come from pharmaceutical interests. Only one would represent an organization of patients living with diabetes.
Some supporters of the bill were disappointed to see a particularly hard-hitting provision removed from the replacement bill passed by the state Senate. The original version of the bill would have directed the task force to research ways to create a free emergency supply of insulin for 30 days, but that provision was removed due to difficulties negotiating with pharmacists, Keizer said. in the Senate committee’s final vote on the bill. January 24.
The provision was inspired by a 2020 Minnesota emergency insulin law, the Alec Smith Insulin Affordability Bill, which provides at least 30 days of insulin to those who need it. an urgent need for $35 or less. Insulin manufacturers must provide it to the program free of charge or face fines.
“The emergency insulin supply was something we were really excited about because it could help people who were uninsured. And, obviously, those people are more likely to be people of color, BIPOC, and older people, right? Johnson said, referring to those who are black, indigenous and of color. “It was a point of fairness here to make sure the uninsured weren’t left out of that equation.”
The bill is heading for a vote in committee on Wednesday.